In the use of diagnostic endoscopy for reflux esophagitis and Barrett's esophagus, what should gastroenterologists be doing but probably aren't? Ask Prateek Sharma, MD.
Dr. Sharma, of the University of Kansas Medical Center, in Kansas City, offered his recommendations on the subject in a lecture at the 2017 Digestive Disease Week.
The primary thing "we should be doing more of" in reflux esophagitis involves proper classification of pathologic changes, he told attendees. "We should be describing this condition using the Los Angeles classification system, and try to avoid terms such as 'mild' and 'severe.' It's not just because it's a new classification system, because it's actually not; it's because the LA grade predicts healing and outcomes of erosive esophagitis."
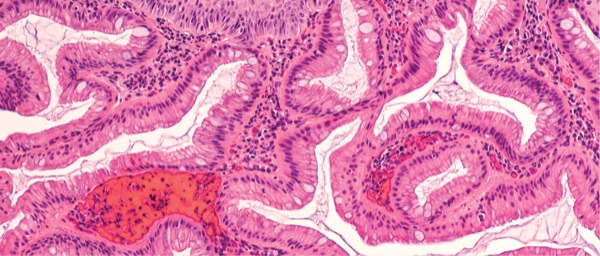
In Barrett's esophagus, two features—columnar-lined esophagus and intestinal metaplasia—point to the diagnosis. After determining that a patient has BE based on these features, gastroenterologists should use standard terminology and avoid descriptions such as "short" and "long" Barrett's segments, Dr. Sharma said.
Specifically, GIs should use the Prague C & M (classification and maximum extent) criteria, which are validated and have high interobserver agreement. For example, Dr. Sharma said, a C2M5 lesion means a Barrett's segment that is 5 cm long with a distal 2-cm circumferential and a 3-cm proximal segment in the form of a tongue. "The use of standardized terminology gives much more information than saying it's a 'long Barrett's.'"
The Prague C & M classification is also linked to patient outcomes, which is important for the utility of any classification system, he noted. In a 2016 analysis of a database of 152 patients with high-grade dysplasia or esophageal adenocarcinoma, the criteria showed that for every 1 cm increase in the extent of Barrett's, the patient's risk for failing endoscopic therapy increased by 30% (P<0.001) (DDW 2016; abstract Sat254). "C & M is linked to outcomes, so it's important to measure the extent of BE," he said.
Equally important is knowing that a slightly irregular Z line—less than 1 cm of columnar metaplasia in the distal esophagus—should not be labeled BE, according to Dr. Sharma. A recent prospective study examined outcomes among 1,791 patients with nondysplastic BE at baseline who had irregular Z lines and intestinal metaplasia (Gastroenterology 2017;152:987-992). After a median follow-up of about five years, none of the patients with irregular Z lines at baseline had developed high-grade dysplasia or esophageal adenocarcinoma. All 71 such cases developed in patients who had BE of 1 cm or longer.
"This is evidence that patients with irregular Z lines do not progress, at least up to five years," Dr. Sharma said. "We don't want to increase the pool of patients with BE who have a very low risk of progression to begin with."
Regarding tissue sampling in BE, Dr. Sharma advised following the Seattle protocol, which directs endoscopists to take four-quadrant biopsies every 2 cm. Ideally, they should use a "turn and suction" technique and take samples only after a thorough inspection of the Barrett's mucosa, he added. "Do we actually do this? Probably not," he said.
Showing the importance of a thorough inspection, Dr. Sharma cited a meta-analysis involving 820 cases of BE-related esophageal adenocarcinoma (Gastroenterology 2016;150:599-607). Researchers at Mayo Clinic reported that 25% of the cancers were diagnosed within one year of the index endoscopy, indicating they were likely missed at the initial examination.

Prateek Sharma, MD
"We are not doing a good job of inspecting the Barrett's segment and are probably not taking the biopsies we should," Dr. Sharma said. "You should spend more time looking at columnar-lined mucosa."
Indeed, more time spent in such inspection pays off, according to a study that found more than a doubling in the identification of high-grade dysplasia and cancer when inspection time was at least seven minutes, versus three to four minutes (Gastrointest Endosc 2012;76:531-538).
"The key is to look more and biopsy less," Dr. Sharma said. "A targeted biopsy gives a bigger bang for the buck than random biopsies."
Narrow band imaging (NBI) should be guided by the clinician's "confidence in and expertise with it," said Dr. Sharma, who added that he uses the technology in his practice.
Dr. Sharma helped to develop and validate an NBI classification system for identifying dysplasia and cancer in patients with BE. When the Barrett's International NBI Group applied its eponymous BING criteria in a "high confidence" setting, its negative predictive value was 95% (Gastroenterology 2016;150:591-598). The BING working group concluded that when images are assessed by clinicians who are well trained in the technology, the system can classify BE with better than 90% accuracy and a high level of interobserver agreement.
"We've been able to show that—at least in the hands of experts—you can rule out high-grade dysplasia and cancer with a very high negative predictive value, and this helps you avoid lots of unnecessary random biopsies," Dr. Sharma said. However, he noted, while clinicians who are "good at it" can use NBI, the current guidelines do not recommend that NBI replace traditional approaches.